In 2012 a review in the International Dental Journal stated botulinum toxin jabs, better known as Botox, were as effective as a mouth guard in reducing the problems of teeth clenching, grinding and the associated pain. That attitude has now reversed and it is even thought to cause tooth loss.
Evidence has recently emerged showing that Botox treatment may trigger a dramatic loss of bone density in the jaw, with parts of the jaw losing up to 40 per cent of bone volume after just one single treatment. What’s more, nobody knows when, or if, the weakened bone will fully regain its strength.
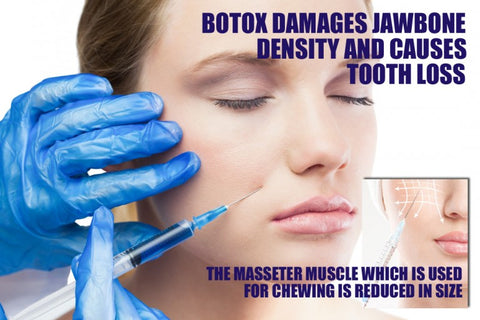
Botox jabs in the jaw are big business today. The paralysing effect is widely used to prevent tooth grinding, and also used by cosmetic doctors to slim the lower face. The treatment reduces the size of the masseter muscles, which are the large chewing muscles located on the jaw in front of the ears, and can cause dramatic cosmetic changes in a matter of weeks.
Teeth grinding, known as Bruxism, not only damages the teeth but can also cause headaches and facial pain, known as temporomandibular joint disorder (TMD) or temporomandibular joint pain (TMJ pain).
Injecting Botox into the masseter muscles means you’re unable to bite down with the same force but the evidence is emerging that the treatment may trigger loss of bone density
One of those leading research in the field is Dr Karen Raphael, professor of oral and maxillofacial pathology at New York University College of Dentistry who became concerned after reading animal studies that showed very dramatic losses in bone density after Botox for was used for these conditions – even after just one single injection of Botox. Researchers found that after only four weeks, the bone in the injected area was ‘severely decreased’. Three months later only half the lost bone had been restored.
Researchers said that in humans this significant degree of bone loss could be ‘a risk factor for fractures’. Normally, changes caused by Botox are assumed to be temporary, but even as early as 2004, doctors noticed that changes to the jaw were long lasting. Yet TMD and facial slimming patients are encouraged to repeat their treatments every 12 weeks.
So how might Botox be linked to bone loss? Our bones are constantly renewed. Old bone is dissolved while cells that are called osteoblasts are making new bone. They produce new bone in response to tugging by muscles and impact. But when masseter activity is reduced by Botox, it can’t push and pull the jaw as powerfully, reducing the amount of bone remodelling and thus bone density, explains Caroline Mills, consultant maxillofacial and facial plastic surgeon at Wexham Park Hospital, Berkshire.
‘A colleague recently saw a patient who had Botox in the masseter for ten years and has discovered her jaw joint is literally melting away.’ This loss of bone in the jaw is linked to an increased risk of loose or lost teeth.
She says the side effects of long-term Botox use in the jaw could include pain, increased risk of jaw fracture and even a need for joint replacement. She says doctors and dentists offer the treatment in good faith but may fail to warn patients of this risk because they themselves are unaware of it.
Six million people in the UK are thought to have Bruxism and should note that a mouth guard worn during sleep is a safer and more effective option to combat the problems and side effects of teeth grinding and clenching.
Allergan, the company that manufactures Botox have now said:
‘It’s important to note that Botox is not approved in the UK for the treatment of bruxism, temporomandibular muscle and joint disorder or for slimming of the lower face. While there are studies exploring the effects of muscle weakening on bone density, the clinical significance of these findings is as yet unclear.’
Allergan is conducting studies exploring the safety and efficacy of Botox when injected into the masseter muscle, the company added.
